Gas Sensors in the Toilet?
Why the Future of Gut Health Is Passive and Personal
Introduction
Millions of people live with digestive discomfort yet rarely talk about it.
Worldwide, 5‑10 % of the population has irritable bowel syndrome (IBS) and those who seek care often wait years for a diagnosis [aboutibs.org].
IBS symptoms are unpredictable – diarrhoea may alternate with constipation and stress can worsen, but not cause, symptoms.
In the United States alone, IBS accounts for 20–40 % of gastroenterology visits, yet patients still struggle with stigma, trial‑and‑error diets and cumbersome symptom diaries.
Thankfully, a new wave of innovations promises to make gut tracking effortless. This article explores why passive, sensor‑based monitoring is on the horizon and how it could empower people with IBS, diverticulitis and other gut conditions.
The gut controls more than digestion
Our intestines are not just pipes; they are a hub where the gut, immune system and brain communicate. Recent research explains that the gut–brain axis consists of bidirectional neural pathways linking the gut and the brain.
Vagal sensory nerves carry signals from the gut to the brain, influencing mental health and wellbeing.
Remarkably, around 95 % of the body’s serotonin – a neurotransmitter involved in mood, sleep and pain perception – is produced in the gut.
Disruptions in this communication pathway can affect not only digestion but also mood and energy, which is why gut disorders often coexist with anxiety or depression. Conventional tracking methods, such as food diaries, help identify triggers but demand constant attention and rarely capture underlying physiological changes.
Why manual tracking falls short
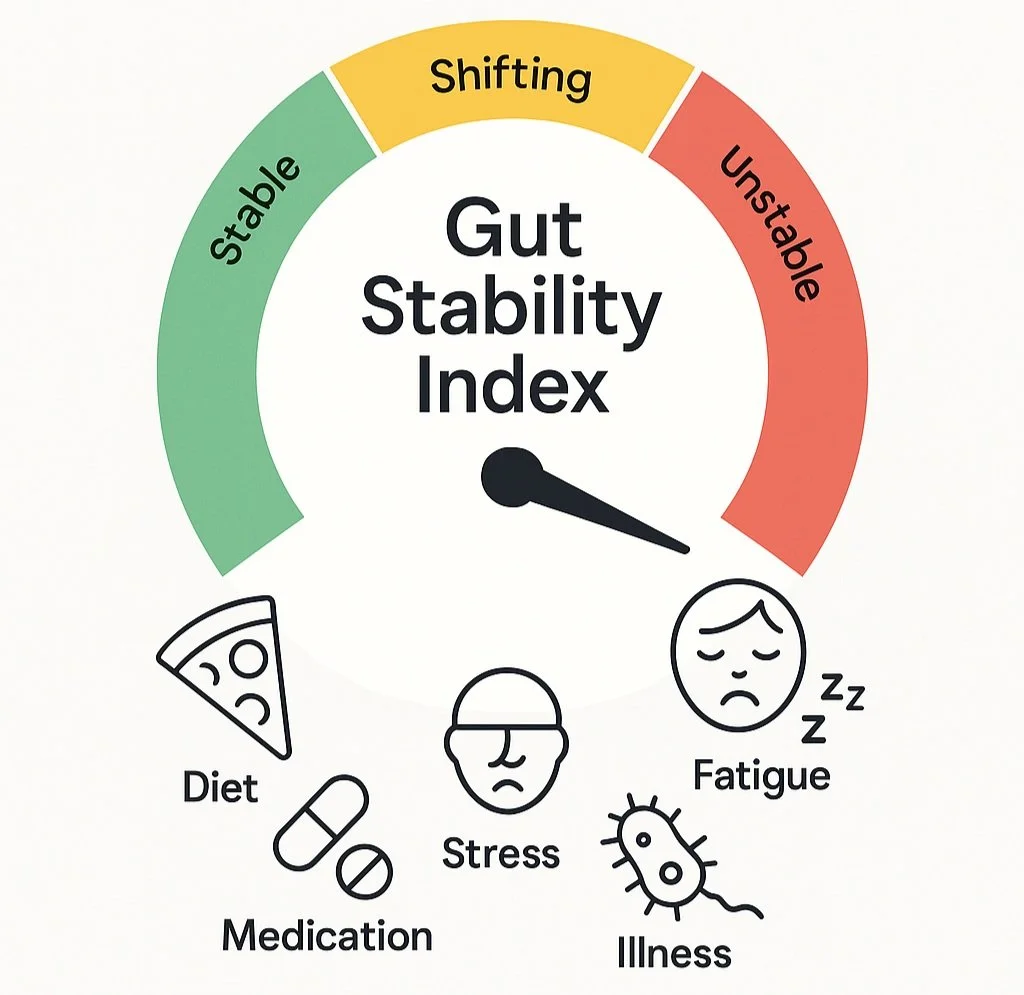
IBS and other functional gut disorders are highly variable; symptoms can change from day to day.
Patients often keep food journals or symptom logs, yet these require meticulous entries and may miss hidden patterns.
Even when people identify triggers (for example high‑FODMAP foods, caffeine or stress), they cannot easily see the biological processes happening in their gut.
Meanwhile, healthcare providers still rely on episodic tests (blood work, stool assays and colonoscopies) that provide only a snapshot. Many patients wait more than six years before receiving an IBS diagnosis.
Clearly, we need tools that can passively collect data and warn us when something is off.
Enter passive gas sensors and smart toilets
Passive monitoring uses sensors that work in the background without user input. Smart toilets are an ideal platform because they can collect urine and stool samples during normal toileting.
Sensors integrated into a toilet seat can measure heart rate, oxygenation and other vital signs, while mechanical arms or sample collectors can capture small quantities of stool or urine for analysis.
Data from urine and stool can reveal early signs of disease such as cancer or metabolic disorders, enabling longitudinal monitoring. Although most commercial “smart toilets” today focus on bidets and seat warmers, researchers at Stanford and Duke universities are developing prototypes that automate sample collection and even quantify stool consistency using computer vision.
Passive monitoring isn’t limited to toilets. A new study from Mount Sinai showed that wearable devices like Apple Watch and Fitbit can predict inflammatory bowel disease (IBD) flare‑ups up to seven weeks in advance. The researchers measured heart‑rate variability, oxygen saturation and daily activity; these metrics changed before participants reported symptoms. Because wearables collect data continuously, they enable remote monitoring and early intervention.
How gas sensors and e‑noses work
Many gut disorders produce volatile organic compounds (VOCs) – gases released by bacteria and human cells. Researchers have found that VOCs spread through blood and are excreted in breath, sweat, urine and stool. These gases form an individual’s “odor fingerprint” and reflect metabolic changes.
An electronic nose (e‑nose) is a device with a sensor array that can detect patterns of VOCs. Compared with traditional lab tests, e‑noses are non‑invasive, rapid and cost‑effective, making them attractive for at‑home health monitoring. The same VOC‑sensing technology is being miniaturized into toilet‑mounted gas sensors and ingestible capsules. By analysing the gases released from your bowel movements, these sensors can infer changes in your microbiome, identify food intolerances or signal impending flare‑ups.
Biohacking goes mainstream
Gut tracking is part of a broader wellness movement. FitBiomics, a microbiome start‑up, predicts that biohacking will become a mainstream wellness trend and the market could reach US$21 billion by 2030. The report notes that accessible practices such as gut health optimization and biological data tracking will be essential for living healthier and longer lives.
People are no longer content with one‑size‑fits‑all solutions; they want personalized insights. Artificial intelligence and data analytics are already helping scientists sift through sensor data to predict flares and tailor interventions.
The IntelliGut vision
At IntelliGut, we believe that monitoring your gut should be as easy as brushing your teeth. Our product is a clip‑on sensor for your toilet that passively analyses gases released during bowel movements. It combines e‑nose technology with machine learning to detect patterns associated with IBS, diverticulitis and other gut conditions – all without asking you to log every meal or handle samples.
What makes IntelliGut different?
Passive and unobtrusive: You simply attach the device to your toilet, and it does the rest.
Personalized insights: By tracking your unique odor fingerprint over time, the system can spot deviations that may signal flare‑ups or dietary triggers.
Data you can trust: Our algorithms are informed by the latest research on VOCs, gut microbiome and wearable data.
Privacy by design: Data is encrypted and stored securely. Only you control who sees your reports.
Looking ahead
Smart toilets and gas sensors are still emerging technologies, and there are challenges to overcome, from data privacy to cost. Yet the potential is enormous. By passively collecting real‑time data, we can move from reactive care to proactive health – identifying problems before they become symptoms, personalizing treatments and even uncovering links between gut health and mental wellbeing.
We’re not offering a cure‑all. Our goal is to empower you with information so you can have better conversations with your doctor and make lifestyle choices that support your gut.
Join the movement
Want to be among the first to try IntelliGut? Join our waitlist and subscribe to our newsletter for gut health tips, product updates and early‑access opportunities.
Remember: Always consult a healthcare professional for medical advice. IntelliGut provides insights, not diagnoses.